Exosome Research in Human Asthma
Bronchial asthma is a chronic inflammatory disease of the airways involving multiple cells and cellular components. Clinical manifestations include recurrent episodes of wheezing, shortness of breath, chest tightness, or cough, accompanied by airway hyperresponsiveness and variable airflow limitation. Inadequate diagnosis and treatment of asthma may result in irreversible airway narrowing and airway remodeling with the prolongation of the disease.
In recent years, the role of exosomes in asthma airway remodeling has received attention. Exosomes are composed of a bilayer phospholipid membrane and biologically active substances such as proteins, lipids, and nucleic acids, which are key carriers for signal transduction and play an important role in organismal physiopathological processes.
Exosomes in the Progression of Asthma
Exosomes are capable of transporting a wide range of elements and are thought to be highly relevant in the asthma process.
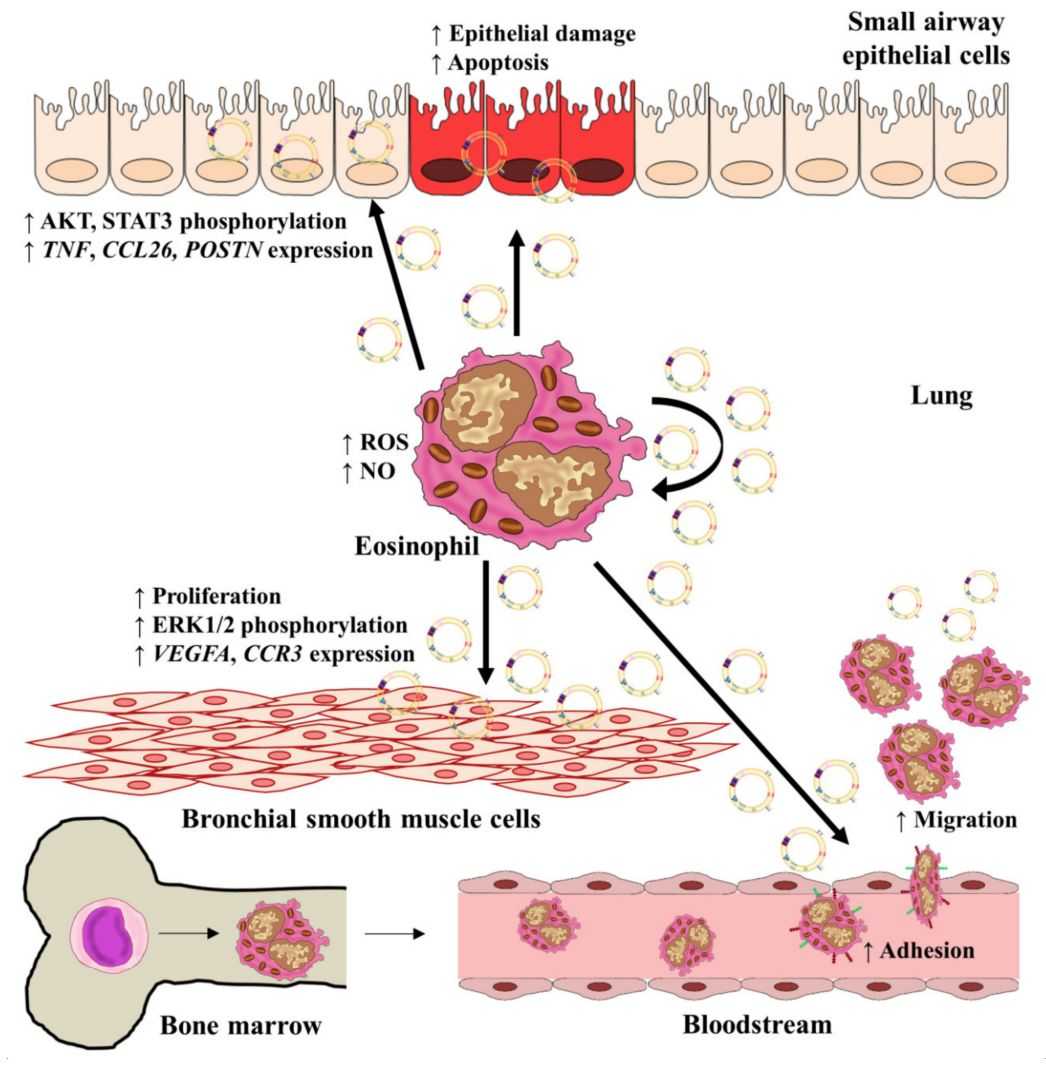 Figure 1. The role of eosinophil-derived exosomes in asthma inflammation. (Cañas JA, et al., 2021)
Figure 1. The role of eosinophil-derived exosomes in asthma inflammation. (Cañas JA, et al., 2021)
- Exosomes and Airway Epithelium
In asthma airway remodeling, structural changes in the airway epithelium include epithelial cell detachment, cilia loss, and mesenchymal transformation. Secretion and transfer of exosomes between airway epithelial cells play an important role in airway biology and epithelial remodeling. Exosomes of fibroblast origin are found to promote airway remodeling by regulating epithelial cell proliferation in patients with severe eosinophilic asthma compared with healthy controls.
- Exosomes and Airway Smooth Muscle
Hyperproliferation and hypertrophy of airway smooth muscle cells are involved in airway wall thickening and airway narrowing, promoting airway remodeling in asthma patients. The results also showed that activated neutrophil-derived CRNDE (Colorectal Tumor Differential Expression of Long-stranded Non-coding RNA) is transferred to airway smooth muscle cells via exosomes and promoted airway smooth muscle cell proliferation and migration through enhanced IKKβ phosphorylation activating the NF-κB pathway.
- Exosomes and Extracellular Matrix
Thickening of the subepithelial layer in asthma is due to excessive deposition of extracellular matrix proteins, which are mainly produced by activated airway smooth muscle cells and fibroblasts. Airway epithelial cells cultured in vitro have been found to secrete the enzymatically active INPP4A via exosomes and transfer it from epithelial cells to fibroblasts or inflammatory cells. INPP4A inhibits fibroblast proliferation and extracellular collagen deposition by inhibiting PI3K/Akt signaling.
- Exosomes and Angiogenesis
Angiogenesis and microvascular changes characterize the chronic inflammatory response in asthma. During the pathogenesis of asthma, the bronchial vasculature may undergo inflammatory changes in the bronchial wall through vasodilation, vascular regeneration, and microvascular leakage. The study observed an increased exosomal component from blood in alveolar lavage fluid, validating the chronic inflammatory response-induced conversion of perivascular cells to myofibroblasts and increased vascular leakage during airway remodeling.
Exosomes in the Diagnosis of Asthma
Exosomal RNA sequencing showed significant differences in the miRNA profiles of exosomes in bronchoalveolar lavage fluid from healthy subjects and asthmatics. These findings provide a new idea for asthma diagnosis. The expression level of serum exosomal miRNA-7b in children with asthma is closely related to the degree of inflammatory response and lung function, which is of clinical value in assisting the assessment of the disease. Compared with healthy controls, miRNA-223 and miRNA-21 levels are significantly increased in patients with moderate asthma, suggesting that both could be considered biomarkers or used in targeted immunotherapy for asthma. In addition, in vitro results showed that the expression of miRNA-125b in serum exosomes positively correlated with the severity of asthma, and the expression level of miRNA-125b in serum exosomes could be used as a noninvasive diagnostic marker for the degree of asthma.
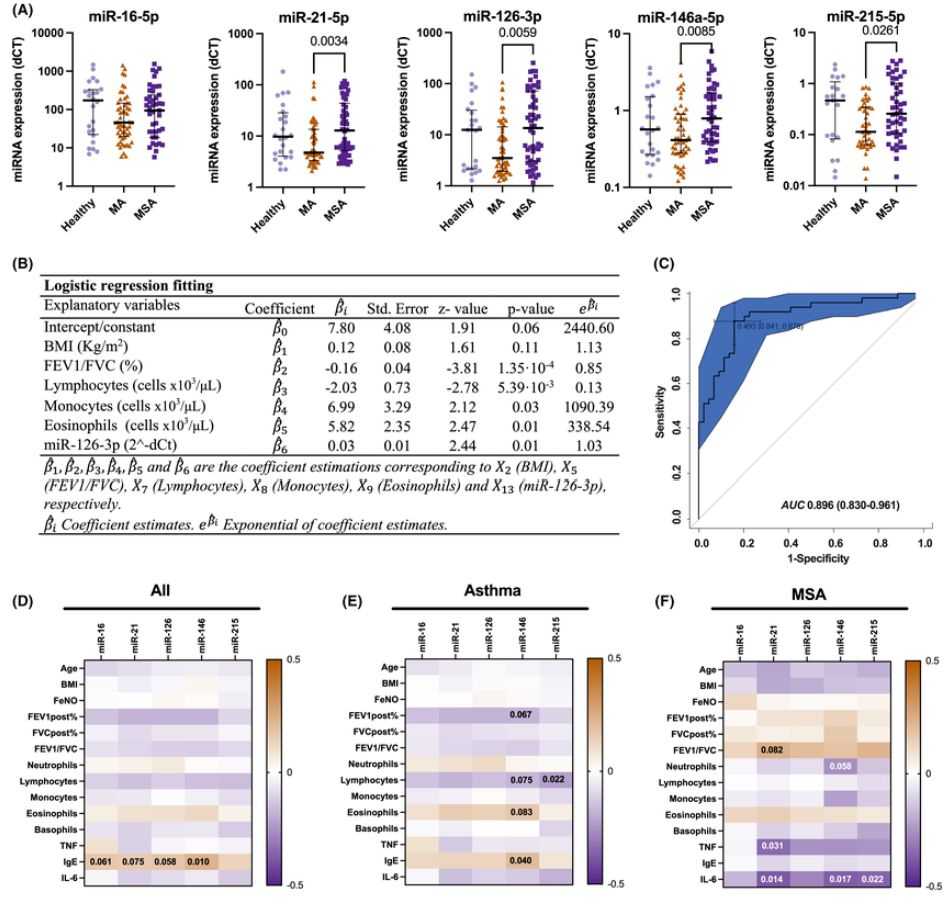 Figure 2. Serum exosomal miRNA expression correlates with asthma severity. (Vázquez-Mera S, et al., 2023)
Figure 2. Serum exosomal miRNA expression correlates with asthma severity. (Vázquez-Mera S, et al., 2023)
Exosomes in the Treatment of Asthma
Most of the current studies on exosomes in asthma diagnosis and treatment have focused on exosomes secreted by adipose stem cells and mesenchymal stem cells. Adipose stem cell-derived exosomes significantly attenuated airway hyperresponsiveness in asthmatic mice and improved allergic airway inflammatory responses. MSC-derived exosomes decreased total alveolar lavage fluid cell and immune cell counts, as well as cuprocyte proliferation and collagen deposition in an animal model of asthma, and are effective in reducing airway inflammatory responses while inhibiting airway remodeling. Under hypoxia, MSC-derived exosomes showed better efficacy in preventing chronic allergic airway remodeling in mice.
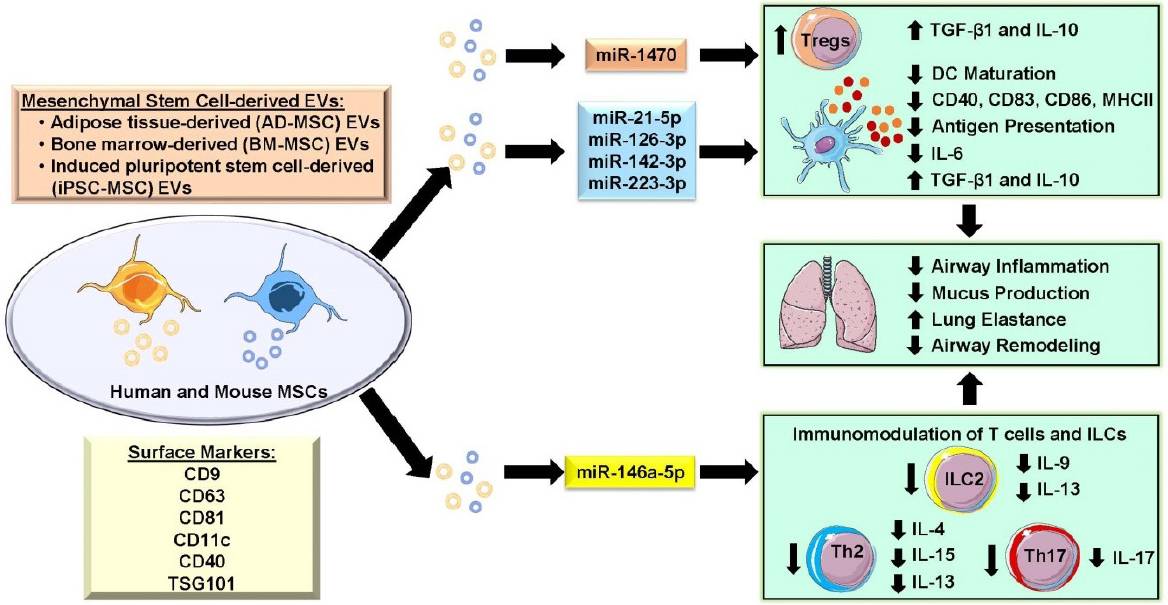 Figure 3. Modulation of mesenchymal stem cell-derived EV in allergic asthma. (Srinivasan A, Sundar IK, 2021)
Figure 3. Modulation of mesenchymal stem cell-derived EV in allergic asthma. (Srinivasan A, Sundar IK, 2021)
| Cat No. | Product Name | Source |
| Exo-HDBF-02 | HQExo™ Exosome-SDH-Asthma plasma | Exosome derived from Single Donor Human Asthma plasma |
| Explore All Exosomes Isolated from Human Asthma Plasma | ||
Exosomes are involved in numerous aspects of airway remodeling in chronic asthma, and exosomes of multiple cellular origins have shown promising results in the diagnosis and treatment of asthma. The advantages of broad stability and modifiability make exosomes promising as markers for asthma diagnosis and new avenues for targeted therapy.
Creative Biostructure provides comprehensive exosome services and high-quality exosome products. If you are interested in our business or have any doubts, please feel free to contact us for more details.
References
- Cañas JA, et al. Exosomes: A Key Piece in Asthmatic Inflammation. International Journal of Molecular Sciences. 2021. 22(2): 963.
- Vázquez-Mera S, et al. Serum exosome inflamma-miRs are surrogate biomarkers for asthma phenotype and severity. Allergy. 2023. 78(1): 141-155.
- Srinivasan A, Sundar IK. Recent updates on the role of extracellular vesicles in the pathogenesis of allergic asthma. Extracellular Vesicles and Circulating Nucleic Acids. 2021. 2(2): 127-47.