At the beginning of the outbreak of the new coronary pneumonia in New York City, Aakriti Gupta, MD, after only a few days of caring for critically ill patients, realized that this is far more than just a respiratory disease.
“I’ve been on the front line from the beginning. I have observed that patients clot a lot, even if they don’t have diabetes, they also have high blood sugar, and many others experience heart and kidney damage,” said Gupta, who is a cardiologist in Colombian cardiology and first deployed to the COVID Intensive Care Unit at Columbia University Irvine Medical Center.
At the beginning of March, there was not much clinical guidance on the non-respiratory effects of COVID-19, so Gupta decided to combine the research results that have just appeared in the literature with the experience of doctors. He and his colleagues reviewed the latest COVID- 19 findings on the effects of the extrapulmonary organ system and provided clinical guidance for doctors. Their review article was recently published in the journal Nature Medicine, entitled Extrapulmonary manifestations of COVID-19, which is the first extensive review of the effects of COVID-19 on all affected organs except the lungs.
“Doctors need to treat COVID-19 as a multi-system disease,” Gupta said. “There is a lot of news about blood coagulation, but it is important to understand that a significant portion of these patients suffer from kidney, heart and brain damage, and doctors need to treat these diseases and respiratory diseases.”
Blood clots, inflammation, and an overactive immune system
Researchers said that in the first few weeks of the pandemic, doctors saw many thrombotic complications than they expected from their experience with other viral diseases. These complications can have a profound impact on the patient.
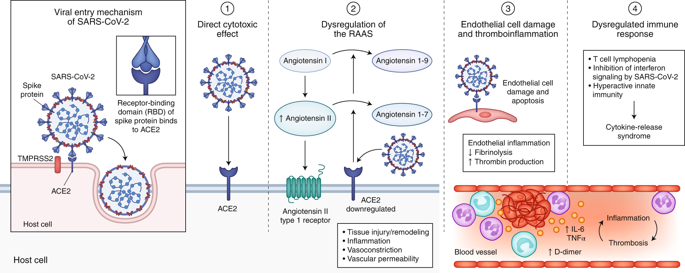
Scientists believe that these coagulation complications may be caused by viruses attacking blood vessel cells. When the virus attacks blood vessel cells, inflammation increases and the blood begins to form large and small clots. These blood clots can flow throughout the body, causing serious damage to organs and perpetuating the vicious cycle of thrombus inflammation.
To combat coagulation and its destructive effects, clinicians at Columbia University are conducting a randomized clinical trial to investigate the optimal dose and timing of anticoagulant drugs for severely ill patients with COVID-19.
This unstable inflammation can also overstimulate the immune system. Although doctors initially avoided using steroids to suppress the immune system completely, a recent clinical trial found that at least one type of steroid-dexamethasone-can make mechanical ventilation necessary. The mortality rate of patients was reduced by a third. Randomized clinical trials for specific components of thrombus inflammation and the immune system (such as interleukin-6 signaling) are ongoing.
Scientists around the world are working at unprecedented speed to understand how this virus hijacks the normally protective biological mechanisms. They hope this will help develop more effective, precise, and safer treatments for COVID-19 in the near future.
Hit the heart
A blood clot can cause a heart attack, but the virus can attack the heart in other ways.
The mechanism of heart damage is currently unclear, because in autopsy cases, the virus is usually not isolated from the heart tissue.
The heart muscle may be destroyed by systemic inflammation and the subsequent release of cytokines. Cytokines are proteins secreted by immune cells that usually clear infected cells, but can get out of control in severe COVID-19 cases.
Although the heart is severely damaged, the need to protect personnel and patients from the spread of the virus prevents doctors from using the diagnostic and treatment strategies commonly used in the early stages of a pandemic, including heart biopsy and cardiac catheterization. With the decline in the prevalence of the disease, this situation has changed.
Renal Failure
Another surprising finding is that the proportion of COVID-19 patients in the ICU is high with acute kidney injury.
The ACE2 receptor used by the virus to enter the cell has a high concentration in the kidney, which may be the cause of kidney damage. Studies in China have reported renal complications, but in New York City, clinicians have found that up to 50% of patients in the ICU have renal failure.
“About 5% to 10% of patients require dialysis. This is a very high number.”
There is currently a lack of data on long-term kidney damage, but a considerable number of patients may require permanent dialysis.
The researchers pointed out: “Follow-up studies on patients with complications during COVID-19 hospitalization will be crucial.”
Nervous system effects
About one-third of patients may experience neurological symptoms, including headache, dizziness, fatigue, and loss of smell.
Even more worrying is that strokes caused by blood clots account for 6% of severe cases and 8% to 9% of delirium.
Patients with COVID-19 can be intubated for 2-3 weeks; a quarter of people need to breathe on a ventilator for 30 days or more. The intubation time is very long and the patient needs a lot of sedatives. Before COVID, ‘ICU delirium’ was a well-known symptom, and this hallucination may not be the effect of a virus, but rather the effect of long-term sedation.
Although physicians have received sub-professional training, they have to keep all organ systems in mind when caring for the patients before them. Researchers hope that their review, observations, and recommendations can help other clinicians in those areas where cases have surged.
Reference
Aakriti Gupta et al, Extrapulmonary manifestations of COVID-19, Nature Medicine (2020). DOI: 10.1038/s41591-020-0968-3